12. Asthma Exacerbations in the Emergency Department or Urgent Care
Asthma exacerbations
Asthma exacerbations are a common cause of respiratory distress. When evaluating a patient with respiratory distress thought to be secondary to asthma, a brief history and physical examination should be conducted concurrently with the prompt initiation of therapy.
History
- Timing of onset of symptoms
- Trigger (if known)
- All current controller and reliever medications including doses, devices prescribed, adherence pattern, recent changes, frequency during current exacerbation, timing of last doses, and perceived response to therapy
- Risk factors for asthma-related death e.g. history of intubation, exacerbation within 30 days
Box 4-1. Factors that increase the risk of asthma-related death
- A history of near-fatal asthma requiring intubation and mechanical ventiation521
- Hospitalization521 or emergency care visit for asthma in the past year
- Currently using or having recently stopped using oral corticosteroids (a marker of event severity)521
- Not currently using inhaled coricosteroids85,521
- Over-use of SABAs, especially use of more than one canister of salbutamol (or equivalent) monthly102,522
- A history of psychiatric disease or psychosocial problems,96
- Poor adherence with asthma medications and/or poor adherence with (or lack of) a written asthma action plan96
- Food allergy in a patient with asthma425,523
Factors that increase the risk of asthma-related death
Summarized from GINA 2020: Table 4-1 pg 113
- A history of near-fatal asthma exacerbation requiring intubation, mechanical ventilation or extracoroporeal membrane oxygenation (ECMO)
- Hospitalization or emergency care visit for asthma in the past year
- Currently using or having recently stopped using oral corticosteroids
- Not currently using inhaled corticosteroids
- Overuse of short acting albuterol (more than 1 cannister of SABA monthly)
- History of psychiatric disease or psychosocial problems/instability
- Poor adherence with asthma medications and/or poor adherence to (or lack of) a written asthma action plan
- Food allergy history
Physical Exam
The severity of asthma exacerbations can range from mild distress to respiratory failure. There are several objective respiratory screening tools available to help assess the severity of respiratory distress; however, of the studies reviewed by the Children’s Mercy Department of Evidence Based Practice in June 2020, none had been studied outside of the institution that developed them. It is unknown if the scores are transferable to other settings. When there is a lack of scientific evidence, standard work should be developed, implemented, and monitored.
- Previously, the Children's Mercy ED used Pediatric Respiratory Assessment Measure (PRAM) to determine asthma severity on presentation and guide decision making on nurse-initiated orders for oral steroids based on PRAM score. In an effort to be more consistent throughout the institution, the Pediatric Asthma Score (PAS) is recommended to be used to assess severity of an asthma exacerbation.
- The Pediatric Asthma Score (PAS) is a validated scoring tool to provide an objective measure of asthma severity. It uses five assessments to classify respiratory distress due to asthma as mild, moderate or severe. When combined with a clinical treatment protocol, the PAS has been shown to reliably decrease length of stay, reduce costs related to asthma management and improve quality of care for children with asthma.1
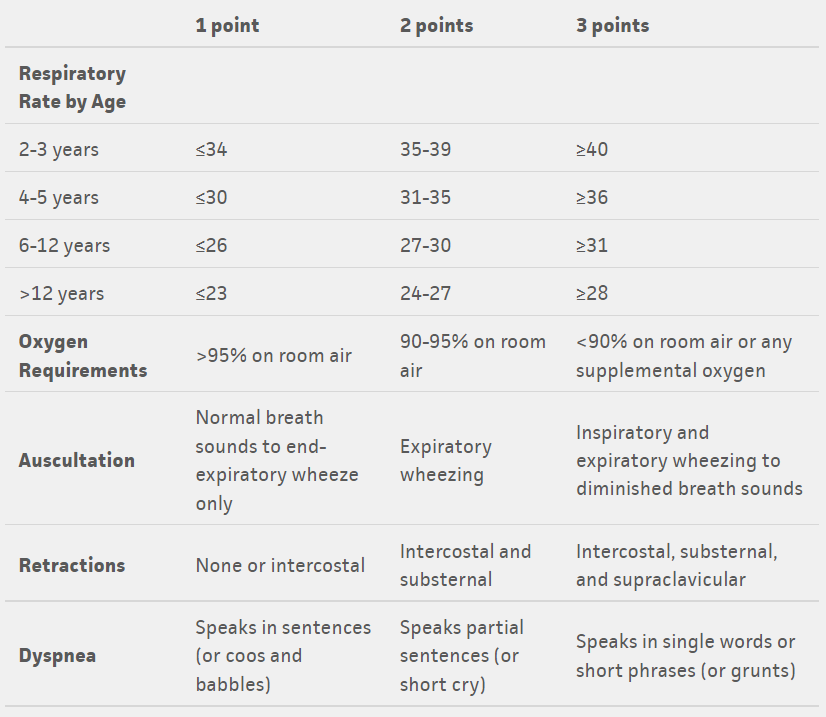

Tables from: https://www.mdcalc.com/pediatric-asthma-score-pas
Treatment in ED/UC
Children’s Mercy has developed clinical practice guidelines for the evaluation and management of asthma exacerbations by location as different locations have access to different resources and can care for patients at different levels of acuity. The Asthma Care Continuum Algorithm considers the asthmatic patient in 4 different locations within our health system emphasizing the need for similar language and treatment as a patient progresses through the health care continuum.
- Link to Asthma Care Continuum Algorithm
- Link to Ambulatory Asthma Exacerbation CPG
- Link to Urgent Care Asthma Exacerbation CPG
- Link to ED Asthma Exacerbation CPG
- Link to Inpatient Asthma Exacerbation CPG
Special considerations for urgent care
Because of many factors including the high acuity of patients requiring IV magnesium sulfate and the risk of hypotension associated with administering magnesium sulfate in a geographically isolated facility, IV magnesium sulfate is not available at Children’s Mercy Urgent Cares.
The ability to provide continuous albuterol is dependent on the staffing or respiratory therapy in the urgent care. Three back-to-back doses of albuterol with ipratropium is similar in dosing to 1 hour of continuous albuterol.
- If patient is significantly improved after 3 back-to-back doses of albuterol where discharge home is likely after a period of observation, patient can continue to be managed in the urgent care.
- If patient is improving but may benefit from additional treatments not available (i.e., IV magnesium), consider transfer to the ED.
- If patient is minimally improved, consider admission via transport.
Special considerations for steroid administration
Corticosteroids PO or (IV if not tolerating PO) should be administered within one hour of arrival for patients with asthma exacerbation so they have time to take effect.
- Short courses of corticosteroids are associated with fewer relapses to additional care, fewer hospitalizations, and less need of beta agonists. Steroids given within the first hour of presentation were significantly less likely to be admitted to the hospital.2
- Literature shows that 1-2 days of dexamethasone (0.6mg/kg/day) have been shown to be equivalent to 5 days prednisone (1-2mg/kg/day).3-5
- Dexamethasone is therefore listed as the preferred systemic steroid for mild to moderate exacerbations in the ED/UCC as it can be administered in a single dose in the ED without need for families to obtain refills of medications after discharge home.
- Severe exacerbations should be treated with IV methylprednisolone as patients may not be able to take medications by mouth and it would be unsafe to administer.
Disposition to home
After treatment and period of observation in the ED, if the patient’s symptoms are resolving, the patient is no longer in respiratory distress, and the family is comfortable continuing care at home they may be discharged from the ED.
- Review asthma action plan with family (this can be done by the respiratory therapist via the order “RT Education” within the ED asthma power plan)
- Ensure patient has sufficient supply of maintenance and/or rescue asthma medications, including the complete course of systemic steroids
- If the patient is not on a controller medication, consider starting one appropriate for patient’s asthma severity on “Steps chart”
- Ensure follow up within one week with a provider, preferably primary asthma provider if available, if not PCP
Disposition to inpatient
If patient’s symptoms are not improving despite interventions or are requiring supplemental oxygen therapy, they should be admitted to the hospital for further management.
- If patient follows in the AAIR clinic for severe refractory asthma (as indicated by a critical information note), they should be admitted to the General Pediatrics service with Pulmonology consult. The pulmonologist on call should also be notified for consultation upon admission.
- If there is a delay to going up to the inpatient units, please ensure the patient continues to receive albuterol therapy at minimum every 2 hours as indicated.
- All other patients can be admitted to general pediatrics.
Considerations for PICU admission
Any of the following criteria would necessitate PICU admission:
- Prolonged continuous albuterol for >4 hrs with worsening symptoms
- Inadequate ventilation with hypercapnea (PCO2 on capillary blood gas >45)
- Need for high flow nasal cannula or non-invasive ventilation
- Persistent hypoxemia (SpO2 <90%) on supplemental O2 (>2 L/min or >50% FiO2 with non rebreather)
- Altered level of consciousness (drowsiness)
- Patients without improvement or with clinical signs of worsening respiratory distress despite maximum therapy in the ED should also be considered for PICU admission
- If there is a delay to going up to the inpatient units, please ensure the patient continues to receive albuterol therapy as indicated
COVID caveats
Nebulized medication is considered an aerosol-generating procedure. Consideration must be given for need compared to inhalers in light of coronavirus-19 precautions.
- Use inhaler medications when clinically appropriate
- In cases where nebulized treatments are needed, all members of the care team should wear appropriate PPE when caring for a patient during and after nebulized treatment
- Appropriate airborne/contact precaution PPE required by all staff when entering rooms for at least the next 70 minutes following the last aerosol generating procedure
When do subspecialists want to be contacted?
If patient and/or family identifies a physician as their primary asthma specialist/doctor, please send a Cerner message to clinic pool or to provider to notify if there are changes to the asthma action plan or if patient needs to be seen for a follow up sooner than anticipated.
- Message pools: Allergy and Asthma Clinic; Pulmonology Clinic (Red or Green Team); AAIR Clinic
Identifying High Risk Asthma Program (HRAP) patients in the ED/UCC prior to discharge
- The High Risk Asthma Program is a program created to identify patients who are high utilizers of health care and/or at high risk for mortality.
- Patients who have had ≥ 4 encounters for asthma at the Urgent Care, ED, or inpatient admission (including the current encounter) within the past 12 months OR was admitted to the PICU for severe asthma exacerbation once in lifetime.
- Patients who have had ≥ 4 encounters for asthma at the Urgent Care, ED, or inpatient admission (including the current encounter) within the past 12 months OR was admitted to the PICU for severe asthma exacerbation once in lifetime.
- Identification of these patients in the ED/UCC prior to discharge allows for appropriate follow-up, but also helps ED/UCC providers know which patients are at greater risk to return to ED for asthma care or at greater risk to have a severe exacerbation.
- Once these patients are identified, an automatic social work consultation and environmental health referral is placed. Patients should also have follow up in a subspecialty clinic for long-term follow up.
- Presently process includes manual review of chart. An automatic process is currently in development.
- If a patient is identified to fulfill the HRAP criteria in the ED/UCC AND if they do not have a subspecialist identified for their asthma care, we recommend a referral to Allergy/Immunology or Pulmonology clinic for long-term asthma care.
Educational point
A first-time diagnosis of asthma should be avoided in the acute care setting especially for first wheezing episode. Patients may be diagnosed with “Wheezing” and/or “Respiratory Distress” but avoid labeling a patient with a chronic diagnosis like “Asthma” or “Reactive Airways” in an acute setting.
- For children <3 years of age, the asthma predictive index (API) is valid if there are 3 or more episodes of wheezing/ year; therefore, first time wheezing episodes does not fulfill criteria.
- Asthma Predictive Index
- Modified Asthma Predictive Index
- Recommend close follow up with patient’s primary care for further evaluation and diagnosis.
- Asthma Predictive Index
- Kelly CS, Andersen CL, Pestian JP, Wenger AD, Finch AB, Strope GL, Luckstead EF. Improved outcomes for hospitalized asthmatic children using a clinical pathway. Ann Allergy Asthma Immunol. 2000 May;84(5):509-16. doi: 10.1016/S1081-1206(10)62514-8. PMID: 10831004.
- Rowe BH, Spooner C, Ducharme FM, Bretzlaff JA, Bota GW. Early emergency department treatment of acute asthma with systemic corticosteroids. Cochrane Database Syst Rev. 2001;(1):CD002178. doi: 10.1002/14651858.CD002178. PMID: 11279756.
- Qureshi F, Zaritsky A, Poirier MP. Comparative efficacy of oral dexamethasone versus oral prednisone in acute pediatric asthma. J Pediatr. 2001 Jul;139(1):20-6. doi: 10.1067/mpd.2001.115021. PMID: 11445789.
- Greenberg RA, Kerby G, Roosevelt GE. A comparison of oral dexamethasone with oral prednisone in pediatric asthma exacerbations treated in the emergency department. Clin Pediatr (Phila). 2008 Oct;47(8):817-23. doi: 10.1177/0009922808316988. Epub 2008 May 8. PMID: 18467673.
- Altamimi S, Robertson G, Jastaniah W, Davey A, Dehghani N, Chen R, Leung K, Colbourne M. Single-dose oral dexamethasone in the emergency management of children with exacerbations of mild to moderate asthma. Pediatr Emerg Care. 2006 Dec;22(12):786-93. doi: 10.1097/01.pec.0000248683.09895.08. PMID: 17198210.
- Asthma Reference Guide Home
- 1. Introduction to Asthma
- 2. Asthma Diagnosis
- 3. Asthma Presentation
- 4. Goals of Asthma Therapy and Management
- 5. Asthma Severity and Asthma Control
- 6. Asthma Outpatient Management
- 7. Treating Modifiable Risk Factors
- 8. Treating Co-Morbid Conditions
- 9. Asthma Medications
- 10. Yellow Zone Therapy Options
- 11. Allergy Immunotherapy and Biologic Therapy
- 12. Asthma Exacerbations in the Emergency Department or Urgent Care
- 13. Special Asthma Considerations for Inpatient
- 14. Asthma Management in the PICU
- 15. Respiratory Support for Asthma Exacerbation
- 16. Asthma Education Resources
